One Health in Action - Emily Jajeh
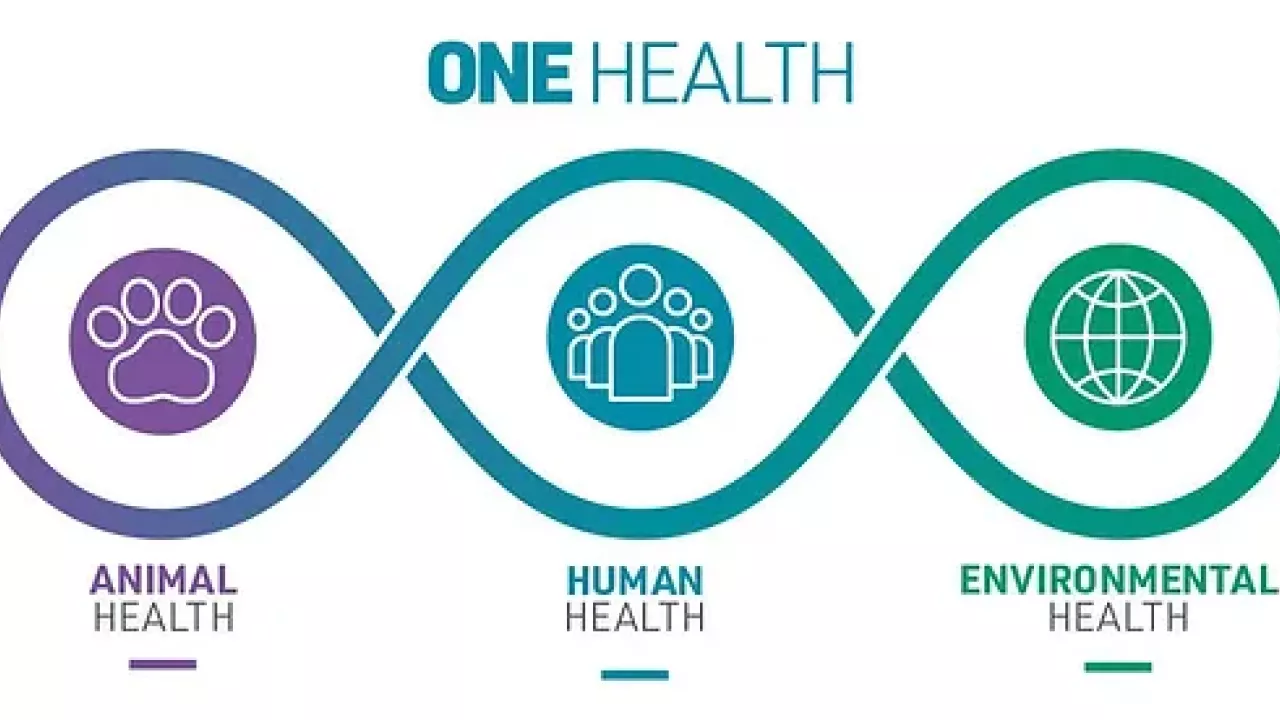
One Health is a central component of the GDB major and having a thorough
understanding of One Health can not only help you in your GDB classes, but will
also help shape your perception of disease control and prevention throughout your
career. One Health is a disease control and prevention approach that recognizes
the connection of the health of people to the health of animals and the environment
(CDC 2024). A One Health approach involves the collaboration of experts from
multiple disciplines working with local leaders, community members, and other
relevant stakeholders to achieve optimal health outcomes. This approach
recognizes the importance of involving the community or population of interest in
the discussion and implementation of disease control strategies. A good One
Health strategy will involve not only medical doctors, biologists, ecologists, and
other scientists, but also community members and leaders. It’s important to
involve the community to ensure that the solutions implemented address the issues
that they feel are the most pertinent, and that those solutions are respectful to
local customs and culture.
understanding of One Health can not only help you in your GDB classes, but will
also help shape your perception of disease control and prevention throughout your
career. One Health is a disease control and prevention approach that recognizes
the connection of the health of people to the health of animals and the environment
(CDC 2024). A One Health approach involves the collaboration of experts from
multiple disciplines working with local leaders, community members, and other
relevant stakeholders to achieve optimal health outcomes. This approach
recognizes the importance of involving the community or population of interest in
the discussion and implementation of disease control strategies. A good One
Health strategy will involve not only medical doctors, biologists, ecologists, and
other scientists, but also community members and leaders. It’s important to
involve the community to ensure that the solutions implemented address the issues
that they feel are the most pertinent, and that those solutions are respectful to
local customs and culture.
There are many examples of disease outbreaks that would benefit from the
implementation of a One Health approach. For example, in 2013-2015, there was
an Ebola outbreak in West Africa (Mwangi, Figueiredo, and Criscitiello 2016). This
outbreak hit the affected West African regions quite hard, largely due to the added
mortality from other neglected tropical diseases that overwhelmed health care
systems. Ebola can be spread from person to person, which contributed to its rapid
spread, but it also can be spread zoonotically, namely from the handling and
consumption of bushmeat. First responders to the outbreak had a clear
understanding of the human-to-human transmission of the disease, but they did not
give as much recognition to the animal-to-human transmission. In addition to the
lack of proper attention towards the zoonotic origin of the disease, the burial rites
practiced by many of the affected communities exposed more people to the virus.
Ebola virus disease (EVD) is a zoonotic disease; bats have been found to be the
main reservoir host, and contact with bats or other infected animals can spread the
virus to humans (Hussein 2023). Human-to-human transmission occurs through
direct contact with bodily fluids. EVD causes flu like symptoms, vomiting, and
diarrhea, and rapidly evolves into a hemorrhagic fever.
The burial traditions practiced in the communities affected by Ebola often involved
close contact with the infected individual’s corpse, which contributed to the spread
of the infection. However, the health workers responding to the outbreak only
considered the health risks of the burial rites and ignored the cultural significance
of the traditional burial practices (Maxmen 2015). The dismissal of local customs
resulted in resistance from affected communities. Community members retaliated
against the health workers disrespecting their burial traditions; for example, some
people would throw stones at ambulance drivers, attack health workers, and hide
their sick relatives in the forest. These retaliation events contributed to the rapid
spread of the disease, and could have been easily avoided by having an open
discourse with local communities and demonstrating respect for their traditions.
For example, in June of 2014, a pregnant Guinean woman died from Ebola. Her
fellow community members insisted that the woman’s fetus must be removed from
her body before burial so as to not disturb the world’s natural cycles. Rather than
force the village to compromise their beliefs and bury the body anyway for the sake
of decreasing the risk of further contact with the virus, they called in an
anthropologist from Cameroon. This anthropologist worked with the villagers to
find a compromise; by communicating with elders in the community, the
anthropologist was able to find a ritual that would both prevent further contact
with the infected corpse and protect the natural cycles from being disrupted.
We can learn from the Ebola outbreak in 2013 and create better strategies to
respond to disease outbreaks in the future. From my experience as a GDB student
and from my experience researching in Africa, it is clear to me that the key to
providing effective, ethical health care interventions is acting with cultural
humility, respect, and openness. The first responses to the 2013 Ebola outbreak
were dismissive and disrespectful of the culture of the communities they were
attempting to help. Their lack of attention towards the importance of earing the
community’s trust and respect made their intervention strategies less effective.
Their strategies would have been more effective and ethical if the One Health
approach was properly employed. A multidisciplinary team would help target the
disease itself and the sectors of health it’s impacting from multiple fronts. For
example, some team members experts in zoology, ecology, and/or wildlife biology
would focus on studying the transmission route from animals to humans, and work
on solutions to controlling that disease pathway. At the same time, public health
specialists, anthropologists, social workers, and community leaders would work
together to understand why people are coming into contact with the animals and
work with the community to form a plan for how they can provide health education
for how to limit interactions with wildlife or interact more safely. On the medical
side, teams of doctors, nurses, and other healthcare workers would work together
as a team with the local leaders and healers to create a plan to treat infected
individuals and limit the risk of further infection. All of these teams, however, will
only be able to promote positive change if they prioritize working with the
community rather than against them. They need to focus on gaining the trust of the
community by listening to their needs and being open to learning new ways to
approach disease control based on the beliefs and customs of the local community.
This involves the aid team being willing to listen and make compromises, and
being open to addressing the crises that the community feels are most important to
address first. Sometimes this looks like working with the community to facilitate a
ritual that will address issues the community feels are most important before
addressing the issues that the aid team feels are most urgent. Showing interest in
and respect for a communities beliefs, values, and traditions builds trust and will
facilitate more open communication between the community members and aid
teams that will result in more effective and sustainable disease control outcomes.
For example, in June of 2014, a pregnant Guinean woman died from Ebola. Her
fellow community members insisted that the woman’s fetus must be removed from
her body before burial so as to not disturb the world’s natural cycles. Rather than
force the village to compromise their beliefs and bury the body anyway for the sake
of decreasing the risk of further contact with the virus, they called in an
anthropologist from Cameroon. This anthropologist worked with the villagers to
find a compromise; by communicating with elders in the community, the
anthropologist was able to find a ritual that would both prevent further contact
with the infected corpse and protect the natural cycles from being disrupted.
We can learn from the Ebola outbreak in 2013 and create better strategies to
respond to disease outbreaks in the future. From my experience as a GDB student
and from my experience researching in Africa, it is clear to me that the key to
providing effective, ethical health care interventions is acting with cultural
humility, respect, and openness. The first responses to the 2013 Ebola outbreak
were dismissive and disrespectful of the culture of the communities they were
attempting to help. Their lack of attention towards the importance of earing the
community’s trust and respect made their intervention strategies less effective.
Their strategies would have been more effective and ethical if the One Health
approach was properly employed. A multidisciplinary team would help target the
disease itself and the sectors of health it’s impacting from multiple fronts. For
example, some team members experts in zoology, ecology, and/or wildlife biology
would focus on studying the transmission route from animals to humans, and work
on solutions to controlling that disease pathway. At the same time, public health
specialists, anthropologists, social workers, and community leaders would work
together to understand why people are coming into contact with the animals and
work with the community to form a plan for how they can provide health education
for how to limit interactions with wildlife or interact more safely. On the medical
side, teams of doctors, nurses, and other healthcare workers would work together
as a team with the local leaders and healers to create a plan to treat infected
individuals and limit the risk of further infection. All of these teams, however, will
only be able to promote positive change if they prioritize working with the
community rather than against them. They need to focus on gaining the trust of the
community by listening to their needs and being open to learning new ways to
approach disease control based on the beliefs and customs of the local community.
This involves the aid team being willing to listen and make compromises, and
being open to addressing the crises that the community feels are most important to
address first. Sometimes this looks like working with the community to facilitate a
ritual that will address issues the community feels are most important before
addressing the issues that the aid team feels are most urgent. Showing interest in
and respect for a communities beliefs, values, and traditions builds trust and will
facilitate more open communication between the community members and aid
teams that will result in more effective and sustainable disease control outcomes.
References
CDC. 2024. “About One Health.” One Health. November 21, 2024.
https://www.cdc.gov/one-
health/about/index.html.
Hussein, Hassan Abdi. 2023. “Brief Review on Ebola Virus Disease and One Health
Approach.” Heliyon 9
(8). https://doi.org/10.1016/j.heliyon.2023.e19036.
Maxmen, Amy. 2015. “How the Fight Against Ebola Tested a Culture’s Traditions.”
National Geographic.
January 30, 2015.
https://www.nationalgeographic.com/adventure/article/150130-ebola-virus-
outbreak-epidemic-sierra-leone-funerals-1.
Mwangi, Waithaka, Paul de Figueiredo, and Michael F. Criscitiello. 2016. “One
Health: Addressing
Global Challenges at the Nexus of Human, Animal, and Environmental
Health.” PLOS Pathogens 12
(9): e1005731. https://doi.org/10.1371/journal.ppat.1005731.
CDC. 2024. “About One Health.” One Health. November 21, 2024.
https://www.cdc.gov/one-
health/about/index.html.
Hussein, Hassan Abdi. 2023. “Brief Review on Ebola Virus Disease and One Health
Approach.” Heliyon 9
(8). https://doi.org/10.1016/j.heliyon.2023.e19036.
Maxmen, Amy. 2015. “How the Fight Against Ebola Tested a Culture’s Traditions.”
National Geographic.
January 30, 2015.
https://www.nationalgeographic.com/adventure/article/150130-ebola-virus-
outbreak-epidemic-sierra-leone-funerals-1.
Mwangi, Waithaka, Paul de Figueiredo, and Michael F. Criscitiello. 2016. “One
Health: Addressing
Global Challenges at the Nexus of Human, Animal, and Environmental
Health.” PLOS Pathogens 12
(9): e1005731. https://doi.org/10.1371/journal.ppat.1005731.
